HIDEF PERFORMANCE BLOG
Return To Sport Testing Post ACLr
By: Tony Trinh, PT, DPT, SCS, CSCS
Injuries to the anterior cruciate ligament (ACL) of the knee are very prevalent in sports, with an estimated 300,000 ACL reconstructions performed annually in just the United States (Greenberg 2018). The most common question every athlete asks after an injury is, “When can I play again?” Every injury and situation is unique. At the end of the day, the answer is “It depends.”
In 2012, Adrian Peterson became the poster child for return to sport after an ACL injury. He defied all odds, running through the NFL on his way to earning league MVP just nine months after sustaining his injury. As a professional athlete, he could dedicate all of his time and resources towards rehabilitation and recovery.
This is a luxury that is not available to probably 99% of the population, but that doesn’t explain all of it. Derrick Rose is also a professional athlete who has a MVP award on his resume, yet it took him almost 18 months to get back on the basketball court.
Return to play decisions require a delicate balance between many factors. Is the athlete safe to return to sport? How quickly can the athlete return, but still minimize risk of reinjury? Does the athlete feel ready to return to sport? Utilizing a criteria-based decision-making model is one way to balance these factors and account for variability in recovery time between athletes.
In this article, we will look at key criteria to decide when athletes are ready to get back in the game.
When Are Athletes Ready to Return to Sport After ACL Reconstruction?
There is no perfect return to sport (RTS) testing battery. However, in a survey of orthopedic surgeons and physical therapists, common factors utilized in return to play decision-making include time, strength, functional testing, and patient-reported outcome measures (Greenberg 2018, 2019).
In fact, Grindem et al. (2016) found that athletes who were able to pass their RTS test battery (including isokinetic quadriceps strength testing, single-legged hop tests, and self-reported outcomes) demonstrated an 84% lower injury rate when compared to those who did not pass their RTS test battery.
Despite the evidence supporting the use of objective RTS testing, Toole et al. (2017) found that amongst young athletes who were already cleared for sport, 44-78% of participants were able to meet individual criterion cutoffs (strength, single-legged hop testing, and self-reported outcome), while only 14% met the cutoff for all criteria.
Let’s review the five main elements that should be included in your RTS testing decision-making process:
-
Quiet knee
-
Strength
-
Functional testing
-
Patient-reported outcome measures
-
Time
Quiet Knee
Before we get into any of the fancy stuff, the first thing that you want to ensure is that you have achieved a quiet knee. What I mean by a quiet knee is a knee that has recovered full range of motion, full quadriceps activation, little to no pain, and no swelling.
Loss of knee motion can lead to increased risk of developing osteoarthritis in the long term (Shelbourne 2012). Knee extension range of motion is especially important, as lacking full extension can have a profound effect on the ability to recruit the quadriceps muscle.
Pain and/or swelling can be a sign that the knee joint is irritated and unable to tolerate the demands of the task. If pain or swelling are present, then return to sport is not advisable.
Strength
Of the individual components of the RTS battery used by Grindem et al. (2016), quadriceps strength was the largest predictor of knee reinjury. They found that with every 1% of improved quadriceps strength symmetry, there was a 3% reduction in reinjury rate.
In the cohort that Toole (2017) investigated, 70-80% of the participants met the cutoff criteria for each individual hop test, but only 43.5% met the cutoff for quadriceps strength. This is consistent with research showing that approximately 20-45% of patients demonstrate appropriate quadriceps strength when they are cleared to return to sport.
Many athletes are cleared to return to sport despite continued deficits in muscle strength and function. The importance of maximizing quadriceps strength after ACL injury cannot be overstated. In fact, we have a separate article all about quadriceps strength and ACL rehab.
Functional Testing
Functional tests can provide useful information when it comes to assessing dynamic stability and power, aiding in the decision-making process. There are many options to choose from when it comes to functional testing. We will only cover hop testing and the Y-Balance Test in this article, and encourage you to include other tests you deem appropriate for your athletes.
Hop Tests
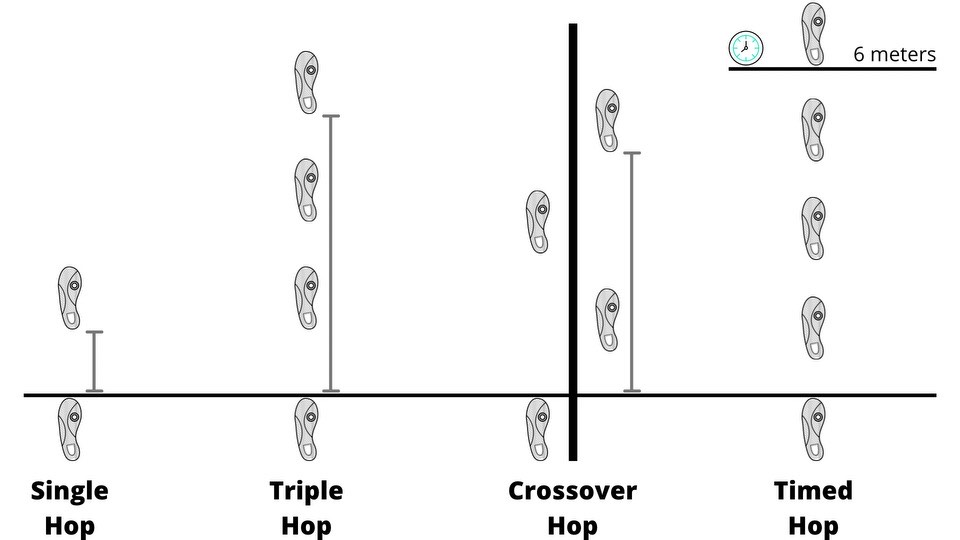
Grindem et al. (2016) and Toole et al. (2017) both used the four different hop tests as a part of their testing battery: single leg hop, triple hop, crossover hop, and 6-meter timed hop. Hop tests were performed on each limb individually and compared between limbs, producing a limb symmetry index (LSI).
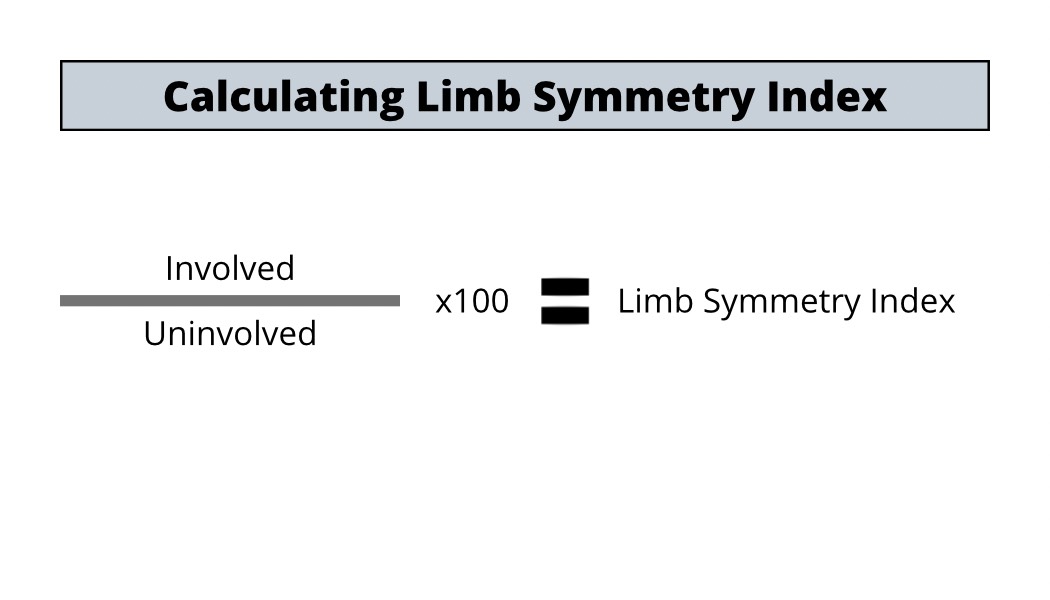
The cut off of 90% LSI is typically used, but a common problem that occurs after injury is that the uninvolved side also becomes deconditioned. Essentially, you could be comparing two flat tires. They might look similar to each other, but you wouldn’t want to take them out on the road. One way to mitigate this is to compare scores to normative data (Myers 2014).
Y-Balance Test
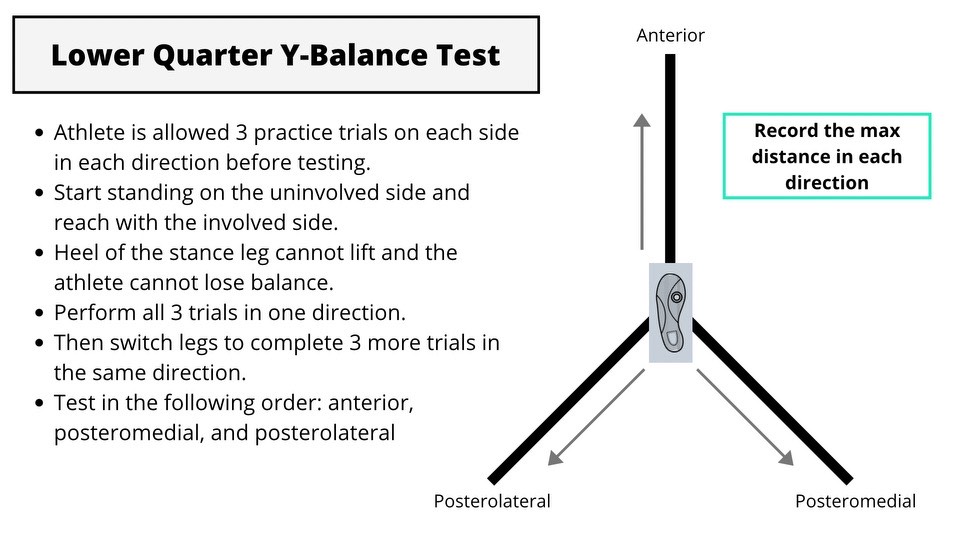
Another test that is commonly used is the Modified Star Excursion Balance Test (Y-Balance Test). This test involves having the athlete standing on one leg and reach as far as they can in three directions (anterior/posterolateral/posteromedial) without losing their balance. Garrison et al. (2015) found that athletes who had >4 cm difference in anterior reach on the Y-Balance Test at 12 weeks post surgery were less likely to achieve 90% LSI for hop testing and quad strength at return to sport.
It is important to understand that all of these tests look at the entire lower extremity as a unit. The knee depends on contributions from the joints above and below (hip and ankle) in order to function appropriately, but that regional interdependence can lead to compensations. These compensations potentially place the athlete at higher risk of injury (Kotsifaki 2020). Compensatory strategies likely contributed to the Nagai et al. (2020) findings that demonstrated hop testing’s tendency to overestimate limb symmetry. See article on limitations of hop testing.
Patient-Reported Outcome Measure
To this point we’ve discussed objective measures to assess the function of the knee/lower extremity. But let’s not forget that the rehab process includes the whole athlete, not just the knee. That’s where patient-reported outcome measures come in.
IKDC
The International Knee Committee Subjective Knee Evaluation Form (IKDC) is a knee-specific measure of symptoms, function, and sports activity (Irrgang 2001). Patients answer questions about how they feel with regards to their symptoms and function. Individuals who returned to preinjury level of sports participation after ACL reconstruction have been shown to score higher than those who did not return to their preinjury level of sports participation (Lentz 2012).
ACL-RSI
The Anterior Cruciate Ligament Return to Sport After Injury (ACL-RSI) scale was created to measure psychological readiness to return to sport following ACL injury (Webster 2008). Patients are asked to respond to questions that relate to three important aspects of return to sport: emotions, confidence in performance, and risk appraisal. A cut off score of 56 points at four months post-op has been shown to predict the ability to return to sport at 12 months (Ardern 2013).
These patient-reported outcome measures can help you to get an idea of how the athlete is feeling about their knee, and can help identify psychological barriers associated with returning to play.
Time
While hitting all of the above benchmarks provides a pretty comprehensive picture on the athlete’s readiness to return to sport, we can’t forget that healing takes time.
The common recommendation people are given following ACL reconstruction is that they should be able to return somewhere between 6-12 months. In the previously mentioned study by Grindem et al. (2016), they found that during the first nine months following surgery, delaying return to sport was significantly associated with a lower rate of reinjury. In fact, for every one month delay in return to sport (up to nine months from surgery), the reinjury rate was reduced by 51%. This may partly be explained by biological healing of the graft.
When someone undergoes an ACL reconstruction, a common belief is that the new graft replaces the old ACL. However, this isn’t entirely true. Grafts are typically harvested from tendons (patellar, hamstring, quad), which have different structural properties than the native ligament that it is attempting to replace.
While the graft does function to maintain the stability of the knee, the graft acts primarily as a scaffolding while the body lays down new fibers that more closely resemble the structural properties of the native ACL. This biological process is known as ligamentization and is composed of distinct phases: early healing, remodeling, and maturation.
The structural integrity of the graft changes as it goes through this process, reaching its presumed weakest point during the extensive remodeling/revascularization phase before it starts to strengthen and approach the levels of the native ACL (Scheffler 2008). Changes in the graft can be observed up to 24 months following surgery (Nagelli and Hewett 2017). A meta-analysis by Pauzenberger et al (2013) summarized the research investigating this phenomenon shown in the graphs below.
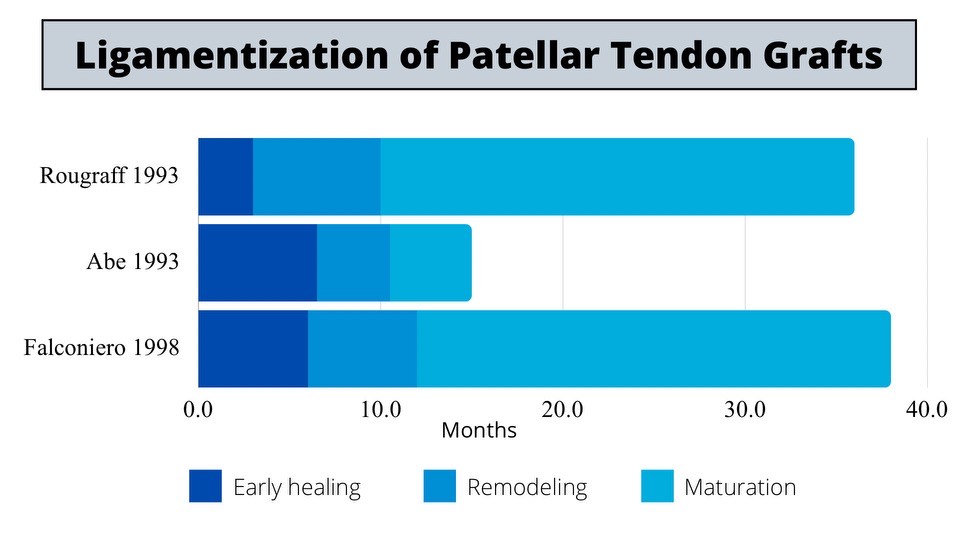
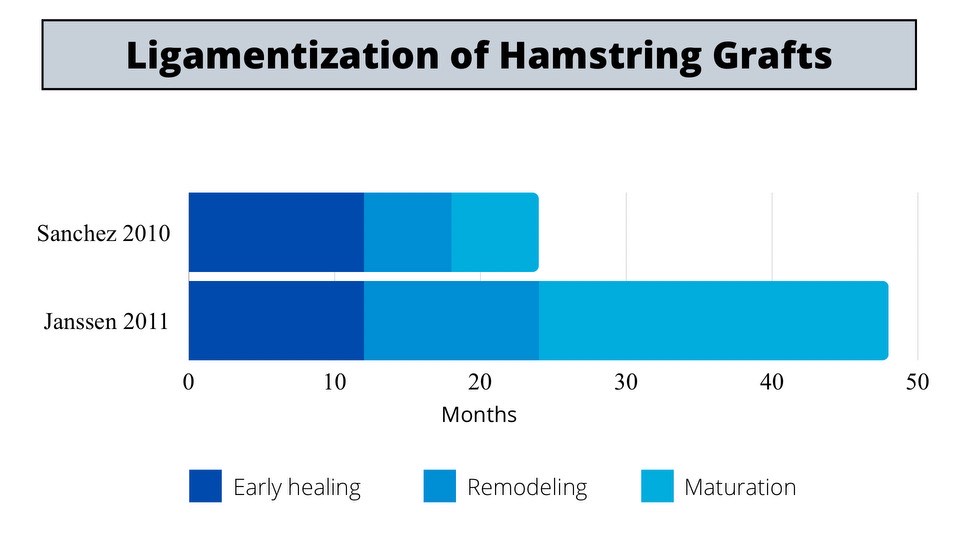
Notice the difference in the ligamentization process between graft types. They undergo the same process, but the hamstring graft may take longer to mature. Direct comparison between these studies is difficult because there is no strict definition to determine phases of the ligamentization process, but it appears graft type needs to be considered in return to sport timelines.
Summary
No single test or metric in isolation will be able to determine when it is safe for someone to return to play following an ACL injury. A criteria-based approach ensures that the simple elements are taken care of before the complex. This decision should be a collaborative effort between the athlete and entire interdisciplinary team while considering the following factors:
-
Quiet knee
-
Strength
-
Functional tests
-
Patient reported outcomes
-
Time
Author: Tony Trinh, PT, DPT, SCS, CSCS
SHARE THIS
COMMENTS